Is the Covid Inquiry about learning lessons or covering backs?
Last month's testimony on masks and airborne spread has left many bemused
This week is the fifth week of testimony in the third module of the covid inquiry. This module is hearing testimony on a range of controversial subjects from the impact on NHS staff, the policy of shielding the most vulnerable and the treatment of long Covid. The government’s handling of each one of these issues has already been subject to much scrutiny in public and many shortcomings have already been identified.
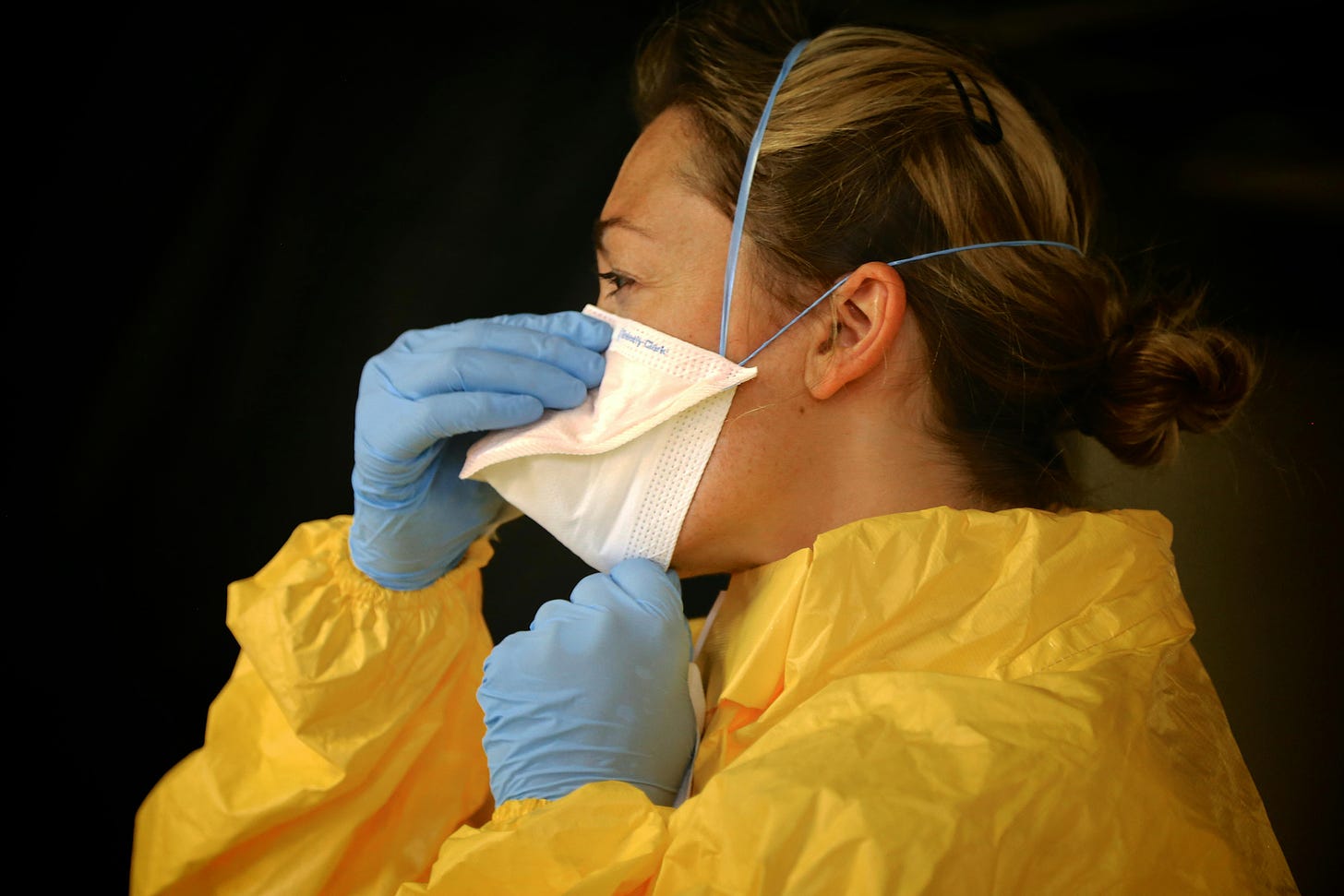
Perhaps the most controversial areas the Inquiry has heard testimony on over the last few weeks are PPE and infection control policy for healthcare workers. On September 18th the inquiry heard contested testimony from chief medical adviser at the UK Health Security Agency (UKHSA), Professor Susan Hopkins.
Perhaps the stand out piece of her testimony was her suggestion that the evidence that high-grade respirators (a type of close fitting mask) known as FFP3s provided better protection to healthcare workers than simple surgical masks was “weak”. Her argument seemed to revolve around the idea that the efficiency of FFP3s - undisputedly shown to be high in ideal laboratory environments - is not borne out in the high-pressure, real-world setting of the covid ward.
A week or so later the Chief Medical Officer Chris Whitty argued along a similar line that “just having kit but no training often produces little or no benefit. The training is fundamental to making the kit useful.” Many mask-sceptics have used these pieces of testimony to argue that the use of respirators by the general public or healthcare workers on the ward was ineffective.
As my co-author, Trish Greenhalgh, and I point out in our recent BMJ rapid response, however, there is substantial evidence to the contrary: that high grade FFP3 respirators can provide up to 100% protection in the ward, whilst staff wearing standard issue surgical masks face a significantly increased risk of catching covid. These are not laboratory-only studies. These are real-world studies demonstrating the effectiveness of these interventions at preventing respiratory infections including covid.
If Hopkin’s testimony goes against much of the available evidence, the natural question that follows is why? Why would the UKHSA ambassador suggest that FFP3s were little better than surgical masks? It has been suggested in some quarters that the official advice from the Public Health England (the predecessor to the UKHSA) and Department of Health and Social Care in the spring and summer of 2020 to wear the less protective surgical mask was based not on the best evidence, but on the government’s inability to source sufficient PPE for its frontline medical workers. It should be pointed out that this is an accusation which the Department of Health and Social care strongly denies, despite the evident lack of appropriate PPE during the early stages of the pandemic.
There have also been suggestions that the Infection Prevention and Control (IPC) cell (members of which from whom the inquiry has also recently heard testimony), charged with creating advice on PPE requirements for healthcare workers, may have laboured under fundamental misunderstandings about the mode of covid transmission. Believing the primary mode of transmission to be large droplets (that fall to the ground quickly) rather than airborne spread through aerosols (tiny droplets that float in the air) may have led the IPC to promote droplet-blocking surgical masks over aerosol-stopping FFP3 respirators. This fundamental misunderstanding may have resulted in the advice that respirators were not necessary.
Fundamentally this inquiry should not primarily be about apportioning blame to those responsible for the sometimes dramatic and often basic mistakes made during the acute phase of the pandemic. Far more important than that is to learn from these mistakes. Admitting mistakes in the PPE guidance and mode of transmission would naturally lead to suggestions that we bolster our stocks of FFP3 respirators and/or our manufacturing capacity in advance of a future airborne pandemic. Understandably, some have suggested Hopkins’ testimony and that of the IPC control cell members is an attempt to cover up previous mistakes in PPE guidance (perhaps caused by a lack of availability of that PPE or a misunderstanding of the transmission mode) rather than to learn lessons from these mistakes to ensure we are better prepared for the next pandemic.




Hi, Kit! I was one of the consultants investigating the first known case in a UK resident - a man who had been on a conference in (I think from memory it was Taiwan), and who had a busy social life. It was clear, from following his secondary and tertiary cases, and their levels of contact, that many had been infected by sharing an indoor space. It was incredibly unlikely that large droplets would have been involved. We looked at spread from people on different parts of a restaurant, and the airflow. I had to stop work for a month or so in February, so was not involved I writing this up. But - if we didn't already know that transmission was mostly or at least frequently airborne from overseas data, we had no excuse for not being confident of this by early February 2020.
It's pretty clear that by framing the testimony in this way they are looking to try and absolve themselves from legal responsibility for disability and death. It's frankly absolutely disgraceful that we're not seeing any really honest reflection on what really happened. Just a series of people trying to cover their arses or protect from wider judgement of institutional failing.